+44 75754 30035 help@rapidassignmenthelp.co.uk
offer
🎁Special Offer 🎁 Discounts - Up to 55% OFF!
🎁Special Offer 🎁 Discounts - Up to 55% OFF!
The social factors defining people's health incredibly affect one's health and the type of health inequality detected. These determinants include socioeconomic status, education attainment, housing and health care. Culture is central to understanding health behaviours, perceptions, and utilisation of services, widening health disparities. Students analyzing these complex public health concepts can benefit from help with assignment writing to structure their arguments effectively and achieve academic excellence. Maternal health is a clear example of how culture plays a significant role in the determinants of health in the United Kingdom.
Inequalities in Maternal Health in the UK
Despite developments in medical care, maternal mortality remains a matter of public health importance in the UK due to ethnic differences. Public Health England statistics indicate that for Black women mortal, the ratio is over forty per one hundred thousand live births as opposed to about eight per one hundred thousand for White women during pregnancy and soon after childbirth (Aveyard and Sharp, 2017). Like African Americans, Asian women also suffer from enormously increased risks that range from between 15 and 20 per 100,000 live births (Edwards, 2020). The above findings depicted a status quo that requires intervention as they show unequal performance between male and female students.
Immanent Cultural Factors or Host Cultural Characteristics
Social demographics are alive to play a role in maternity health inequalities in the UK. Languages are another concern, as most minority ethnic women have language problems in obtaining appropriate and prompt health care (Edwards, 2020). Unfortunate breakdown of communication between patients and their caregivers results in missing antenatal visits or failure to adhere to medical advice given throughout the prenatal period and increasing risks during childbirth. Cultural perceptions of health also dictate the behaviours of the mother-to-be (Hutchings, 2019). For instance, some women rely on herbal remedies or cultural practices of childbirth rather than seeking professional help, thus missing critical moments for intervention. Besides, the individual issues are amplified by systemic bias within the frameworks of healthcare systems.
Social Determinants Influence
This work also ascertains that demographic factors, including poverty, education and housing, significantly affect maternal risk. Low-income women experience the challenge of accessing adequate quality health care mainly because the cost of transport, child care, and actual health facilities is high. Lack of formal education and health literacy Maguire (2011) further makes it difficult for these women to seek appropriate prenatal and postnatal medical care; crowded as well as damp housing also negatively affects health among these women during pregnancy (Hutchings, 2019). All these factors put together cause ethnic minority groups to experience higher maternal mortality than the other groups.
Data Trends and Disparities
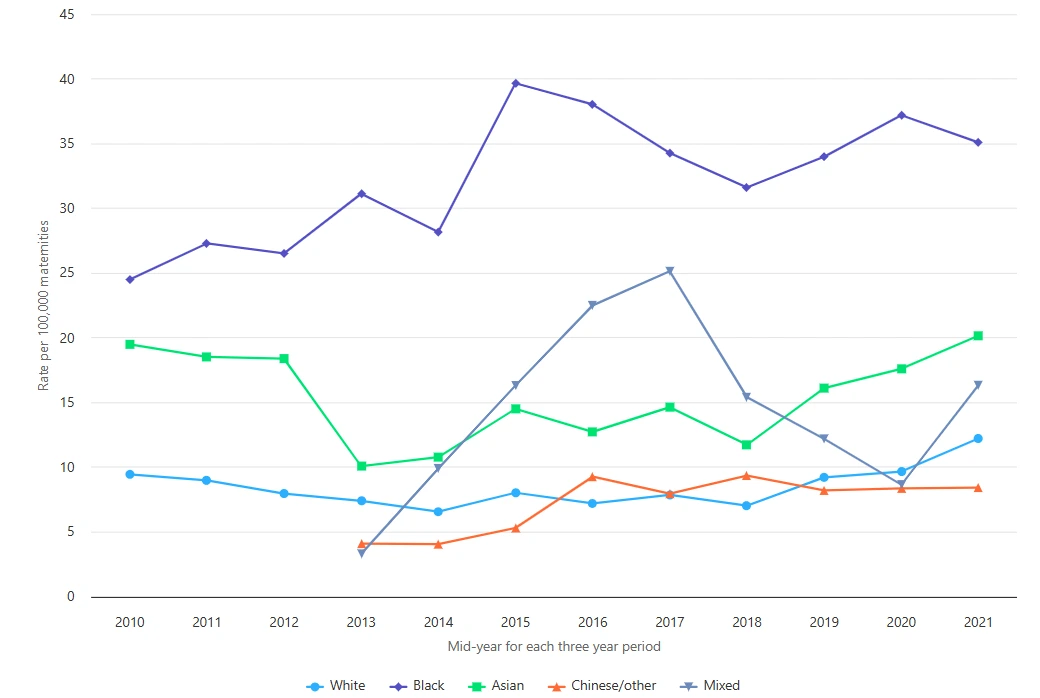
Figure 1: Maternal mortality rates in England
Statistics obtained from Public Health England describe the degree of differences in maternal mortality rates. Currently, Black women top the rates, and they have not changed much in the past years. All ethnicities revealed only minor improvements, albeit Asian women and Black women continued to experience a comparatively high risk while White women had the lowest risk of all (MBRRACE-UK, 2024). This pattern indicates the general trends in the provision of maternal care in Uthe K and underscores the need to address the research findings.
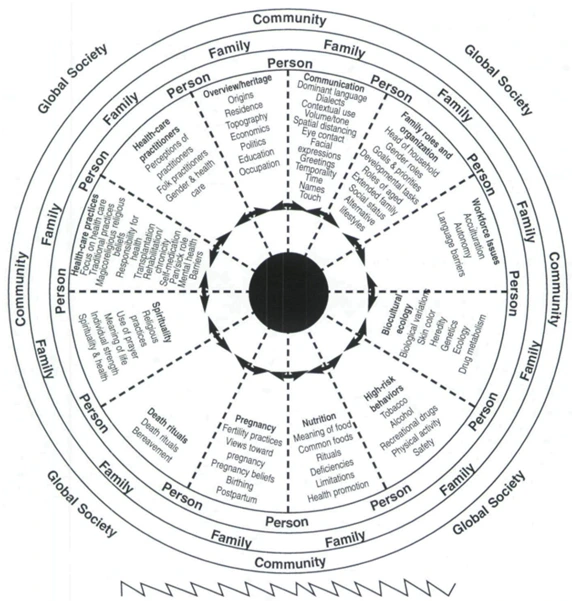
Figure 2: PURNELL'S MODEL
Understanding the root of the Purnell Model
The Purnell Model for Cultural Competence is an extensive framework that aims to assist healthcare practitioners in providing culturally appropriate care. It focuses more on the cross-cultural aspects of care in personal, professional, organizational and international contexts (Purnell, 2005). The model is based on 12 cultural subdomains, which enshrine significant components of cultural self-identity and behaviour patterns.
Relevance to Maternal Health
Explaining disparities in maternal health calls for the use of the Purnell Model to realize that cultural factors among communicating intra and extrapersonal themes significantly affect maternal outcomes. Language differences or culture-related misunderstandings contribute to different forms of delayed or inadequate care (Pandey et al., 2021).
Focus on Two Domains
Communication Domain
The communication domain is essential for WHO’s efforts to undertake language and cultural differences in maternity care. Failure to communicate effectively between the healthcare providers and patients results in delays or even compromised quality of care (Minnican and O’Toole, 2020). For instance, via interpreters, women LEP patients are likely to understate or inadequately explain symptoms or worry about themselves; clinicians are likely to discount or overlook sure illness signs or to delay diagnosis and treatment.
Healthcare Practices Domain
The practices related to the healthcare domain are aimed at learning and appreciating cultural values and norms regarding health. In maternal health, cultural practices of birth and practices after delivery or postnatal practices affect a woman’s management. The Purnell Model can be used herein to create care plans that honour these practices while promoting the safety of the woman and her unborn child (Edwards, 2020).
Get assistance from our PROFESSIONAL ASSIGNMENT WRITERS to receive 100% assured AI-free and high-quality documents on time, ensuring an A+ grade in all subjects.
Practical Applications in the United Kingdom
The Purnell Model of culturally competent care has gradually been implemented in the UK, and healthcare providers are embracing culturally sensitive measures (Edwards, 2020). Measures incorporated involve offering diversity awareness as continuing professional development for health workers and creating minority-targeted health care services.
The UK’s Maternity Transformation Programme aims to tackle maternal health inequalities through strategies like the “Better Births” model, focusing on the Continuity of the Community Midwife Service and culturally sensitive antenatal education for women (Taylor et al., 2022). These include increasing trust, communicating and preventing risk, and enhancing outcomes for high-risk groups, including ethnic minorities. Many differences persist, suggesting that there is a call for large-scale change.
Cultural Interpreter Services used in Norway offer a more general approach to meeting the needs of both immigrant and minority groups. These interpreters bring language and culture into play, improving clients’ communication and the quality of care they receive. Perinatal care is a significant aspect of improving maternal health in the Norway system of care delivery with a low mortality rate among all the population groups (Taylor et al., 2022).
Thus, whereas the UK practice involves targeted interventions directly related to conditions in particular communities, systemic integration in Norway offers more generalised equity. Conceptions from both models are that direct outreach needs to work hand in hand with overall cultural competence to enhance women's ability to receive optimum maternal care(MBRRACE-UK, 2024).
Conclusion
Maternal health disparities vary from one culture to another and from one society to another; therefore, the role of cultural and social determinants of health must be well understood to tackle this challenge. The Purnell Model for Cultural Competence is useful for orientation on how best to offer culturally appropriate care concerning language and tradition. The analysis of the Maternity Transformation Programme targeted at the UK and Cultural Interpreter Services concerned with Norway shows the advantages and drawbacks of each model.
References
This poster showcases the statistics on maternal health, the cultural and social differences in the rate of maternal mortality in the UK, and how different public health interventions seek to overcome such a difference. This paper establishes that ethnic disparities in MM ratios continue in the UK by comparing the groups despite these ongoing frameworks. A study conducted by PHE reveals that black mothers in the UK have a maternal mortality ratio of over 40 per 100,000 live births, which is more than four times that for white women (MBRRACE-UK, 2024). Asian women of child-bearing age also die in relatively high-risk ratios, between 15 and 20 women to 100,000 live births. On the other hand, white women throughout the same age group record relatively lower mortality at about 8 per 100,000 ladies, further highlighting disparities in healthcare provision (MBRRACE-UK, 2024).
Language issues and cultural beliefs are some of the reasons that lead to these inequalities. For example, a patient with cognitive impairment or hearing loss may be unable to understand medical advice in English or their native language (Aveyard and Sharp, 2017). Many Belizean people rely on traditional health practices, which are part of their culture. These may work counter to what their physicians tell them, and such a move may only worsen health outcomes as everyone waits for traditional cures to work. These sources of stress, in combination with racism and discrimination, mean that there is no trust in healthcare, which inhibits health service use (Aveyard and Sharp, 2017). Famine, income difference, housing and education play a role in the health of ethnic minorities, and all these aggravate the outcomes of maternal health among the population.
The PHE data fire the starting shot for the discussion as the healthcare progress revealed by the Maternal Department does not show progressive enhancements in the health of Black and Asian women (Public Health England, 2023). The data trends indicate that much effort has been made to raise disparate access within the targeted campaign. More work must be done to foster fairness and effect structural reforms towards building equitable health systems.
On the other hand, maternal health outcomes in Norway show the improvement that comes with systematically implementing cultural competence to eliminate differences. In Norway's universal health care policy, Cultural Interpreter Services have been integrated to meet all language and cultural barriers (Edwards, 2020). Interpreters guarantee a clear understanding of the information given to immigrants and Minority patients and enhance their confidence in the care delivered by healthcare providers. These trends prove the effectiveness of the systemic approach used in Norway because its data always indicates low maternal mortality figures for all ethnic groups (Purnell, 2005). Through neutral provision of care throughout pregnancy, thereby impacting pregnancy care services, Norway shows that cultural competence can be integrated into the health care system.
The observation that is successfully done in this paper involves analyzing the relative advantages of the UK and Norwegian models. UK initiatives like the Maternity Transformation Programme are targeted at high-risk populations and community-based activities, which are more effective in tackling local population-level variability (Hutchings, 2019). Nonetheless, the relatively stable disparities in the results for Black and Asian females suggest that more fundamental structural transformations are required.
References
These disparities are a result of cultural and socioeconomic determinants, therefore requiring culturally sensitive care.
These statistics profile the ethnic minorities as bearing a higher load. These disparities result from cultural factors such as language, cultural beliefs and structural factors in healthcare organizations. Socio-economic factors also come into play and so appropriately qualify as key considerations. Minore, 2013 states that many women in low-income households face challenges accessing proper health care because of costs, geographical location and low levels of health literacy. All of these reasons help to make ethnic minority women have even worse health conditions in pregnancy and childbirth, which further entrenches inequality.
The activity of the communication domain is based on the conductive problem: language separation and lack of understanding between the caretakers and patients. For instance, providing trained interpreters and culturally appropriate health information can facilitate the comprehension of medical advice details and enhance choice-making among non-English speaking individuals. In health care practices, cultural rights are highlighted in preserving cultures about health and childbirth. For example, some cultures prefer home treatments or distinct childbirth processes that do not conform to medical advice.
It has successfully established rapport and responded to the demands of ethnic minority women.In addition, community referral programs include culturally appropriate antenatal care to help women with language or cultural differences. However, while the above-focused approaches have increased the patients’ satisfaction and involvement, equality is still a concern, showing the tendency of a non–Semic method.
Cultural Interpreter Services of Norway provides service all year round and avails the service to everyone, including those holding private parties. These interpreters are part of the integrated universal healthcare system and quickly help to eliminate language and cultural barriers because these are often immigrant and non-majority populations.
A universal approach inherent in the Norwegian educational system guarantees the homogeneity of cultural competence across the country and applies to all groups of patients. This means that this systemic approach has been highly successful in minimizing disparities but may also not necessarily easily cater to specific needs peculiar to a particular minority group. The key lessons emerging from the comparison are identified. The analysis shows that the UK may need to incorporate systemic cultural competence into its current and future NCSPs. At the same time, Norway might be advised to develop specific cultural-logical mobilization activities related to people with exceptional needs. Therefore, the integration of both strategies presents the right direction in the realization of health equity.
Conclusion
At the same time, the Norwegian Cultural Interpreter Services, similar to a Community Health Promotion Programme, ensures everyone is considered. Through integrating systemic integration with targeted outreach, healthcare systems can decrease disparity, thus improving maternal care on a global scale.
References (PPT)
Introduction to The Design of Buildings Assignment Sample The design of the building is crucial for urban living and creating a...View and Download
Introduction This report demonstrates the application of networking concepts by completing three tasks: developing IP schemes,...View and Download
Introduction to Individual Rights And Identity Assignment Sample In this section, a detailed discussion will be done on...View and Download
Introduction Get free samples written by our top-notch subject experts when you choose Online Assignment Help for reliable and...View and Download
Introduction - LC460 Wellbeing in Society Assignment Sample Wellbeing comprehends quality of life [QoL] and potential of...View and Download
1. Introduction: The Foundation of Organizational Awareness in Schools Get Assignment Helper Services to enhance your...View and Download
